A groundbreaking artificial intelligence-based approach is transforming the ability to predict the risk of cardiac arrest, potentially saving lives by identifying patients at risk of sudden death from cardiac arrhythmias. Developed by researchers at Johns Hopkins University, this new AI technology significantly enhances physicians’ ability to assess risks and could revolutionize clinical decision-making in the management of heart disease, one of the most deadly and perplexing conditions in medicine.
The research, published in Nature Cardiovascular Research, is led by senior author Natalia Trayanova, a professor of biomedical engineering and medicine. “Sudden cardiac death caused by arrhythmia accounts for up to 20% of all deaths worldwide, yet we still have little understanding of why it happens or how to predict who is at risk,” Trayanova explained. “Some patients receive unnecessary defibrillators, while others who truly need them are not getting treatment. Our algorithm aims to accurately predict not only who is at risk but also when a cardiac event is likely to occur, giving doctors the tools to take the right actions.”
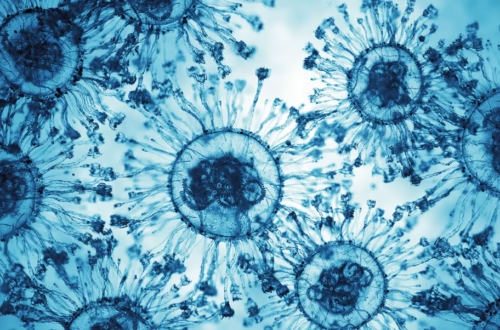
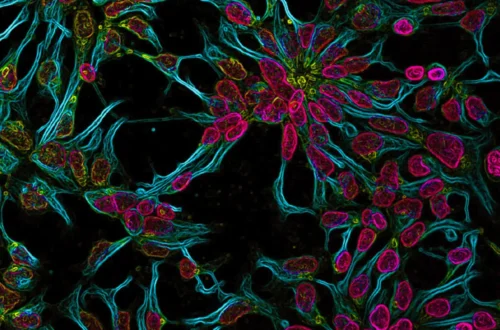
This team is the first to apply neural networks to create personalized survival assessments for heart disease patients. Their AI model, called the Survival Study of Cardiac Arrhythmia Risk (SSCAR), analyzes images of heart scarring, a major contributor to lethal arrhythmias. By using contrast-enhanced cardiac images from hundreds of real patients, the algorithm identifies hidden patterns in the scarring that are invisible to the human eye but crucial for assessing patient risk.
Current methods of analyzing cardiac images only focus on basic scar features such as volume and mass, but these metrics fail to capture the full picture. “The images contain critical information that doctors have not been able to access before,” said first author Dan Popescu, a former doctoral student at Johns Hopkins. “Scar tissue distribution plays a vital role in predicting a patient’s survival chance, and we can now extract meaningful data from these images.”
The researchers also trained a second neural network using a decade of standard clinical data, including factors like age, weight, race, and prescription drug use. By combining both imaging and patient data, the SSCAR model outperformed doctors’ predictions in every measure. Tests using an independent cohort of patients from 60 health centers across the U.S. confirmed the platform’s accuracy and potential for broad adoption, regardless of cardiac history or imaging differences.
“This could dramatically impact clinical decision-making regarding arrhythmia risk and is a key step in bringing patient trajectory predictions into the age of AI,” said Trayanova. “This represents the merging of artificial intelligence, engineering, and medicine, which will define the future of healthcare.”
The team is now working to expand this deep-learning technology to detect other cardiac diseases, and Trayanova believes the approach could be adapted for use in other medical fields that rely on visual diagnosis, marking the beginning of a new era in personalized healthcare.
Subscribe to our newsletter!